Abstract
Introduction:
Thalassemia is characterized by an ineffective erythropoiesis (IE). Increased exposure of phosphatidylserine (PS) on red blood cell (RBC) surface following membrane injury by free radical generation is an important pathway of IE triggering apoptotic signal, which is also associated with hypercoagulable state of thalassemia.
The current study aimed to assess PS exposure on RBC surface using annexin-V as a surrogate marker comparing thalassemic patients with healthy controls based on different clinical & laboratory parameters.
Methods:
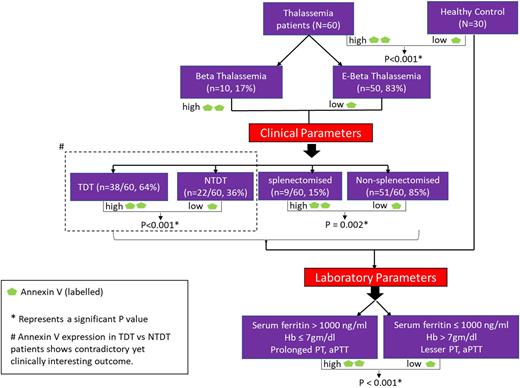
The assay was based on flowcytometric detection using FITC-conjugated annexin-V antibody for PS exposure and PC-7 conjugated glycophorin A for RBC identification. The study cohort consisted of 60 Thalassemia patients including Beta (10, 17%) and E-Beta (50, 83%), attending Department of Haematology at NRS Medical College & Hospital, Kolkata, India between March 2020 to December 2021 and matched healthy controls (n= 30). Patients were broadly segregated based on age, sex, Thalassaemia type (Beta/E-Beta), transfusion dependent (TDT) / Non-transfusion dependent (NTDT) and splenectomy status.
Enrolled patient and control population were assessed for PS exposure using flow cytometer from Navios EX, Beckman Coulter and its correlation with clinical parameters like transfusion dependence, thrombotic episodes, splenectomy status; as well as laboratory parameters including hemoglobin (Hb) level, prothrombin time (PT), activated partial thromboplastin time (aPTT), fibrinogen, serum ferritin level. These were assessed using a battery of statistical tools. Independent t test and Mann-Whitney U test were done for two groups and ANOVA for more than two groups. Qualitative variables were correlated using Chi-Square test. Multivariate linear regression was used to analyze the correlation between multiple variables. P-value <0.05 was considered as statistically significant.
Result:
The median annexin expression was significantly high (P<0.001) in thalassemia patients with Beta (18.15%) and E-Beta (9.2%), compared to control (0.4%) although the difference was not significant between Beta and E-Beta. Similarly, a significant difference (P<0.001) in annexin-V expression was observed in TDT (18%) compared to NTDT (5.4%) as well as in splenectomised (23%; IQR 19.3-28) and non-splenectomised (8.1%; IQR 4.2-18.3) groups (P=0.002). The TDT patients showed a significant risk of iron overload characterized as serum ferritin >1000 ng/ml (37/38, 97.4%) as compared to NTDT (3/22, 13.7%), and also associated with significantly increased annexin expression (18% vs 5.4%, P<0.001). Comparable observations were obtained for pooled thalassemic population with significantly low Hb, prolonged PT and aPTT (Hb: 7.2 ± 1.3 gm/dl, PT: 17.4 ± 4.4 sec, aPTT: 45.6 ± 24.9 sec) compared to healthy control (Hb: 12.6 ± 0.7 gm/dl, PT: 12.6 ± 0.8 sec, aPTT: 26.6 ± 1.9 sec). Similar variations were also significant between TDT & NTDT. The former observation was in concordance to annexin expression as well showing significantly high (P<0.001) annexin-V expression in individuals with low hemoglobin ≤7 gm/dl, prolonged PT and aPTT. Significant annexin expression was not observed with fibrinogen level and no obvious clinical manifestations of hypercoagulability in any patients were detected.
Conclusion:
Therefore, it can be said that RBC PS exposure was significantly high in Thalassaemia patients and it is associated with degree of anemia, transfusion dependence, iron overload, prolonged PT / aPTT and splenectomy status. There is no significant difference in PS expression between E-Beta and Beta population. But contrary to the available literature annexin expression was more in TDT compared to NTDT patients in our study. This discrepancy might be due to suboptimal transfusions in TDT patients leading to inadequate suppression of ineffective erythropoiesis and incomplete replacement of damaged RBCs by healthy erythrocytes. Studies involving larger population are needed to validate this observation.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal